European regulators have delivered a decisive verdict on Oxbryta, the once-promising sickle cell disease medication. On October 17, 2025, the European Medicines Agency (EMA) confirmed that Oxbryta’s marketing authorization will remain suspended across the European Union after reviewing what they say is troubling new safety data.
The decision follows interim emergency measures taken in September 2024, when regulators temporarily halted the drug to assess emerging evidence suggesting a higher rate of deaths and disease complications among patients receiving Oxbryta compared with placebo treatments.
After months of review, EMA’s Committee for Medicinal Products for Human Use (CHMP) concluded that Oxbryta’s benefit-risk balance is no longer favorable, a determination that effectively keeps the drug unavailable for prescription throughout the EU.
What Is Oxbryta and Why Was It Approved?
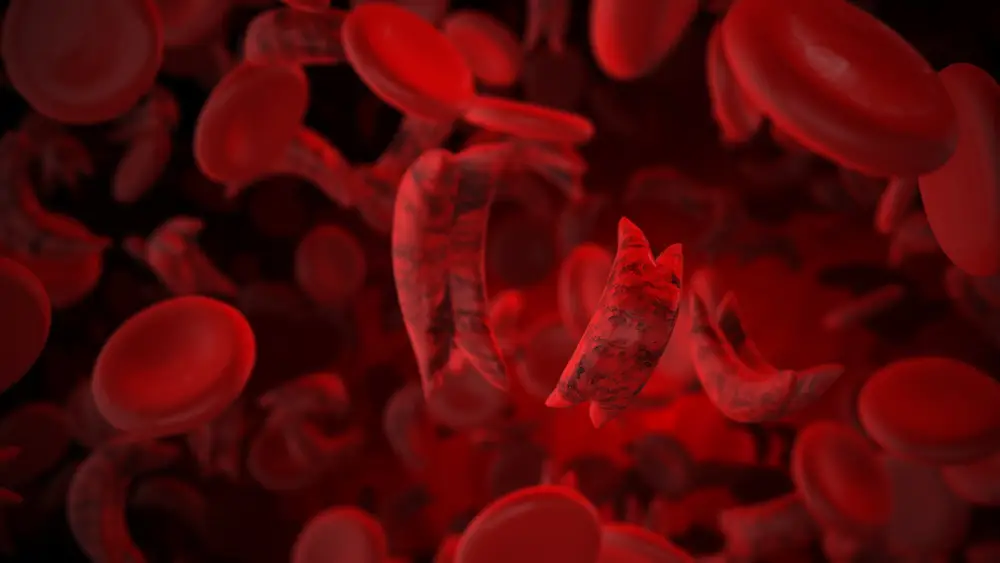
Oxbryta, known generically as voxelotor, was developed by Global Blood Therapeutics and later acquired by Pfizer. The drug was designed to treat hemolytic anemia in patients with sickle cell disease, a genetic blood disorder that affects millions worldwide.
Sickle cell disease causes red blood cells to become rigid and crescent-shaped, restricting blood flow and leading to severe pain, organ damage, infections, and stroke. Oxbryta allegedly worked by increasing hemoglobin’s ability to bind oxygen, theoretically reducing the sickling of red blood cells.
The drug received accelerated approvals based on early clinical data suggesting improvements in hemoglobin levels. In Europe, it was authorized in February 2022 for patients aged 12 and older, either alone or alongside hydroxycarbamide (hydroxyurea).
What New Evidence Triggered the EMA Suspension?
The EMA’s decision centers on recent clinical trials and post-authorization data that painted a far different safety picture than earlier studies.
According to the agency, two major trials raised red flags:
- HOPE Kids 2 trial (GBT440-032): Among children at higher risk of stroke, 8 patients treated with Oxbryta died, compared with 2 deaths in the placebo group.
- RESOLVE trial (leg ulcer study): One patient died during the initial 12-week placebo-controlled phase while receiving Oxbryta. During the subsequent phase, when all participants received Oxbryta, 8 additional deaths were reported.
Across both studies, regulators also observed higher rates of sudden severe pain episodes, including vaso-occlusive crises (VOCs), in patients treated with Oxbryta.
These findings sharply contradicted earlier trials that supported the drug’s approval and showed no meaningful statistical difference in serious outcomes between treatment groups.
Why Regulators Could Not Mitigate the Risks
One of the most consequential aspects of the EMA’s ruling is what regulators say they could not determine.
After consulting external experts, patient representatives, and the EMA’s safety committee (PRAC), the CHMP concluded:
- The mechanism behind the increased deaths remains unclear
- No reliable risk-minimization strategies could be identified
- No patient subgroup could be identified for whom the benefits clearly outweighed the risks
Without a clear explanation or path forward, regulators determined that continuing access to Oxbryta posed unacceptable uncertainty for patients.
As a result, the drug will remain suspended indefinitely while the European Commission prepares a legally binding final decision applicable to all EU member states.
What This Means for Sickle Cell Patients in Europe
The EMA has advised healthcare professionals that Oxbryta should no longer be prescribed, and patients currently taking the medication should be transitioned to alternative therapies.
For patients and families, the suspension underscores the ongoing challenges of treating sickle cell disease safely and effectively. While Oxbryta once represented a novel approach to treatment, regulators now emphasize caution over innovation when safety signals cannot be explained or controlled.
Patients are encouraged to speak with their hematologists about established treatment options such as hydroxyurea, transfusion therapy, and emerging gene-based approaches currently under investigation.
A Broader Regulatory Reckoning
The Oxbryta decision highlights the growing tension between accelerated drug approvals and long-term patient safety.
Regulators across Europe and the United States are increasingly scrutinizing drugs approved through fast-track pathways, particularly when post-market studies reveal outcomes that differ from early trial results.
For sickle cell disease, a condition with limited treatment options, the suspension is both sobering and instructive. It underscores the importance of robust long-term data, transparency, and cautious optimism when evaluating breakthrough therapies.
Looking Ahead
Oxbryta’s suspension does not mark the end of innovation in sickle cell treatment, but it does serve as a reminder that regulatory approval is not the final chapter in a drug’s safety story.
As research continues into gene therapy, bone marrow transplantation, and next-generation medications, regulators say patient safety must remain paramount, even when the need for new treatments is urgent.



Add Comment